Though not extensively discussed sensory processing difficulties can negatively impact emotional regulation in individuals with Post-Traumatic Stress Disorder (PTSD). October 10th is both Sensory Processing Awareness month and World Mental Health Awareness day, making it a good time to consider the relationship between sensory processing disorders and PTSD.

Sensory processing disorders are more common in individuals with PTSD due to its influences on the sensory systems and arousal levels that provide the foundation for self-control. Many individuals who have PTSD struggle with sensory processing, becoming over-aroused or under-aroused in response to minimal sensory stimulation. People with PTSD and sensory hyper-arousal become upset more easily and for longer periods of time by their sensory and emotional triggers. Over reactive hyper-arousal is related to neurological differences that make it more likely to be upset by and harder to get use to sensory input and return to a calm alert state (Green et al., 2015). Mental health therapists depict the challenges of maintaining a calm alert state in PTSD as a limited Window of Tolerance (Teicher et al., 2016).
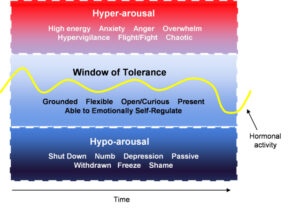
The first step in managing problematic arousal levels is becoming aware of our current arousal level so we can notice when we begin getting hyper or lethargic. The Alert, Zones of Regulation, ARC Energy level, and Traffic light programs are good for helping school students become aware of and manage their arousal levels. Because it’s difficult for some students to be shown different programs, I developed the Arousal Level Strategy that is consistent with all the programs Click FAB Arousal Level Strategy
Sensory-Based Interventions (SBIs) can be developed by occupational therapists with individuals who have PTSD, to help them manage arousal levels for improved self-control. SBIs are individualized environmental adaptations and sensory coping strategies that improve sensory processing and self-regulation. Examples of SBIs include sensory coping areas, movement breaks, mindfulness activities, noise canceling headphones, and positioning a student’s desk further from peers to minimize distractions (Dunn et al., 2016). SBIs can be used to help reduce and respond to dysregulating triggers. Basic Blogpost on SBIs Improved ability to maintain a calm alert state can improve functional skills. Advanced SBI in school Blogpost
Difficulties managing their sensory triggers and arousal levels can negative impact self-regulation in individuals with PTSD. Sensory-based interventions developed with an occupational therapist can provide strategies to enhance self-control for improved functioning.
References
Dunn W, Little L, Dean E, Robertson S, Evans B. The state of the science on sensory factors and their impact on daily life in children: A scoping review. OTJR. 2016;36(2_Suppl:3S-26S).
Green SA; Hernandez L, Tottenham N, Krasileva, K, Bookheimer SY, Dapretto M.Neurobiology of sensory overresponsivity in youth with Autism Spectrum Disorders. JAMA Psychiatry. 2015;72(8):786.
Teicher MH, Samson JA, Anderson CM, Ohashi K. The effects of childhood maltreatment on brain structure, function and connectivity. Nature Reviews Neuroscience. 2016 Oct;17(10):652
