STRATEGIES®
STRATEGIES®
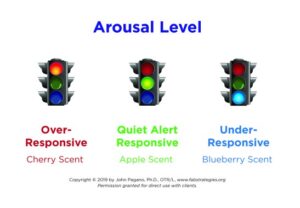
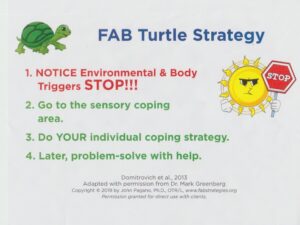
John Pagano, Ph.D., OTR/L


 Half-price Extended Limited Time SALE $2.50 for my e-book HERE
Half-price Extended Limited Time SALE $2.50 for my e-book HERE
See Kirkus Reviews FAB Strategies book review
FREE PREVIEW of my FAB Strategies paperback book on AMAZON
Bookstores and libraries order paperback HERE
Register Now for my April 18 & 19, 2024 Live Online BER Teachers & Therapists TRAIN-the-TRAINERS course for 3-21 year old students BER Train Brochure 2024 Also offered on demand!
Most POPULAR Site Blogpost Sensory Strategies to Improve Behavior HERE
Newest Blogpost CLICK New Interoceptive Awareness Strategies for School Occupational Therapy”
Play my free 90-minute Webinar on School OT Treatment for Students with PTSD HERE
I presented conversations that matter at the AOTA Inspire 2023 Conference about Revitalizing Pediatric OT Mental Health


2023OTPedMHConvthatmatterHandout2023
BERHandoutsVirtualPreKKPres2023
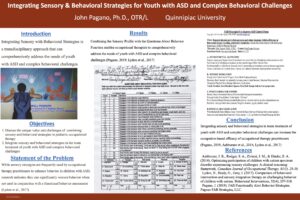
I presented my poster at the 2023 AOTA conference about Occupational Therapy Integrating Sensory & Behavioral Strategies for Youth with Autism Spectrum and Complex Behavioral Disorders

Thanks for reading my FAB Strategies book, I’d appreciate your opinion by leaving a REVIEW
Click New & Trending Blogposts Here: My OT Journey and recent Montana Trainers Conference HERE
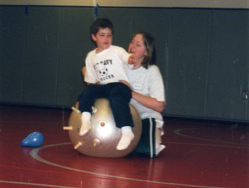
Sensory-Based interventions (SBIs) improve behavior
My free Video Channel is www.youtube.com/@PaganoFABStrategies